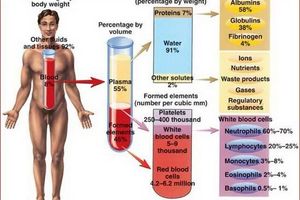
It is known that the use of one's own blood for the treatment of various diseases began in ancient times, that is, since the inception of medicine. Currently, the use of platelet-rich plasma (PRP, PRP) is one of the most successful areas of tissue engineering and cell therapy in medicine. In the evolution of terminology, there are many different names for platelet-rich plasma as an end product. In clinical practice, it is believed that the stimulating effect of platelet-rich plasma is possible when the platelet concentration in it is at least 1,000,000 / μl. When tissue is damaged, platelets play a huge role in tissue healing and regeneration through the release of growth factors. Growth factors are natural polypeptides that have a wide biological local effect on many chicks by influencing the main links of the regenerative process: chemotaxis, cell proliferation, cell migration, differentiation, restructuring, and angiogenesis.
PRP contains such growth factors as: PDGF - platelet growth factor, TGF-β - transforming growth factor, EGF - epithelial growth factor, VEGF - vascular endothelial growth factor, but also adhesive molecules (fibrin, fibronectin and vitronectin), cytokines. During centrifugation, the resulting plasma contains proteins, fibrinogen, nutrients (glucose, lipids), hormones, vitamins, enzymes, intermediate and final metabolic products, inorganic ions, which are involved in the cascade of tissue regeneration [12, 20].
Considering that OLT is an integral part of the patient's own blood, its advantage is that there is no risk of parenteral transmission of HIV infection, viral hepatitis, or the occurrence of immune reactions.
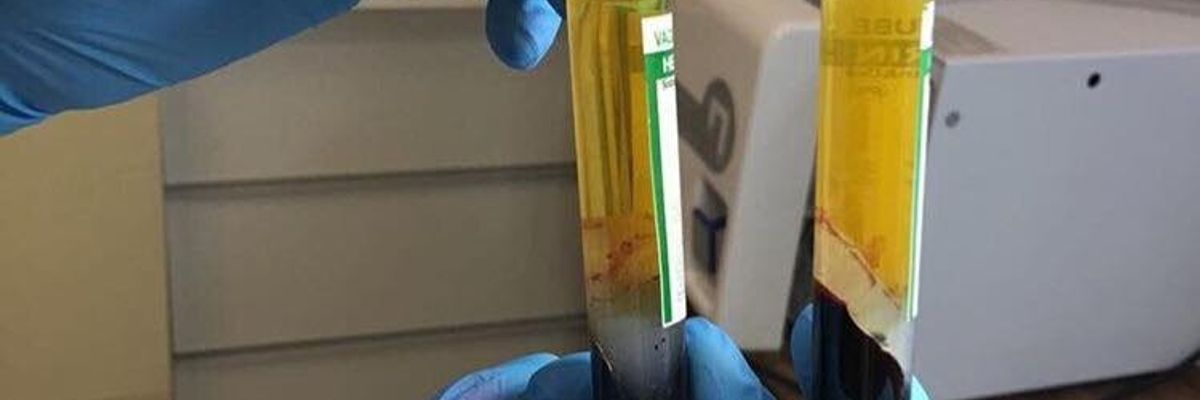
There are various protocols for obtaining PRP by centrifuging whole blood in 1 or 2 stages, after or without the addition of an anticoagulant, to obtain different end products [12, 20].
Currently, there is a simple classification based on the characteristics of fibrin molecules and the content of cells (mainly leukocytes), in which 4 main groups are distinguished: 1) pure platelet-rich plasma (P-PRP); 2) platelet and leukocyte-rich plasma (L-PRP); 3) pure platelet-rich fibrin (P-PRF); 4) platelet and leukocyte rich fibrin (L-PRF). These 4 groups have different methods of obtaining, mechanisms of action, corresponding to the field of application [20].
There are researchers' opinions that many parameters for obtaining PRP, such as the number of revolutions and the duration of centrifugation, were chosen empirically and it is not possible to evaluate their results objectively in comparison with others [20].
A number of authors [17] found that the concentration of platelets in PRP correlated with the number of platelets in the donor's whole blood. However, no statistically significant correlation was found between the number of platelets in PRP and in the donor's whole blood. A significant, but not clinically significant, influence of the sex of the subjects on the platelet concentration was found. No effect of age was found.
When using PRP, a number of researchers had a discussion about the possible influence of its cellular composition. For example, some authors argue that the presence of leukocytes when injected with PRP can negatively affect clinical outcomes due to the risk of stimulating the inflammatory process [31]. Other authors dispute this view and speak of the production of pain mediators and the action of leukocytes with natural anti-inflammatory ability as a regulator of the healing process [31, 33].
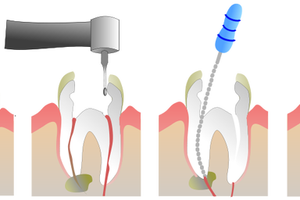
OTP found the greatest application in dental implantology [2]. Thus, the use of PRP for bone grafting and prevention of jaw atrophy before dental implantation, the authors achieved the formation of bone tissue in the early stages [4]. combined with autologous bone transplantation and various bone substitute materials [21, 29, 30].
One of the main mechanisms of regeneration is increased blood supply in tissues by stimulating angiogenesis during the destruction of platelets and the release of growth factors by them. In PRP, these polypeptide growth factors are found in biologically predetermined ratios.
In maxillofacial reconstructive medicine, a gel made from platelet autoplasma and L-PRF membranes are successfully used, including in children with congenital clefts of the upper lip and palate [18, 24].
Platelet-rich plasma has found wide application in periodontology [18].
An injection method for local stimulation of regenerative processes using OTP, obtained after centrifugation in Plasmolifting TM tubes, is described. The study proved the regenerative properties of PRP in the form of a decrease in the degree of inflammation, a decrease in the number of inflammatory cell infiltrates and inflammatory cells in the focus of inflammation of the gum tissue [11].
Numerous studies aimed at studying the effectiveness of the use of PRP in cardiovascular surgery have proven its positive effect in patients after cardiac surgery. Reinfusion of autologous platelet-rich plasma improves hemostasis after cardiopulmonary bypass, can reduce blood loss, perform surgery without transfusion of homologous blood, and also arrest a number of hematological disorders [16, 19, 21].
The observation of severe clinically manifested fibrous dysplasia of the fronto-orbital region, which was reconstructed using OLT, was described [26]. Long-term remission of symptoms and early bone formation were achieved. Combining PRP with allograft or comminuted bone graft is a safe, simple treatment.
The results of clinical studies in abdominal surgery have confirmed the effectiveness of glue with a high content of fibrin in Lichtenstein plastic surgery in patients with coagulopathies associated with liver diseases, as well as those who have been receiving anticoagulants for a long time. ...
The results of an experimental histological study of the structural and functional organization during the healing of aseptic wounds of soft tissues against the background of the use of PRP showed that this method of treatment stimulates the processes of collagenesis, epidermisation, vascularization, and a more rapid scar formation occurs [10].
In their practice, PRP is successfully used in surgical and conservative treatments for inflammatory diseases of the joints [23, 27].
On an artificially created model of osteoarthritis of the knee joint in rats, intra-articular injection of platelet gel was used [23], as well as in works on the treatment of soft tissue injuries of the musculoskeletal system (tears of ligaments, muscles, tendons, tendopathies), the use of PRP in the form of the main, as well as additional therapies (after surgery) are being questioned.
According to L. Yu. Shirokova et al. (2012) observed significant improvements in the functional state of the knee joints with local application of PRP in patients with gonarthrosis with initial manifestations of osteoarthritis. In typical stages II-III gonarthrosis, confirmed by X-ray, OLT has a short-term positive effect only in the first month of observation, whereas in severe gonarthrosis complicated by synovitis, treatment is ineffective.
Intra-articular administration of PRP in an experimental model of a defect in the articular surface of the knee joint in rabbits has a stimulating effect on the regeneration of hyaline cartilage, improving both its qualitative and quantitative characteristics [14].
Of particular interest is the use of OLT end products in aesthetic plastic surgery [25].
There are publications on the use of PRP in otorhinolaryngology to stimulate the regeneration of the tympanic membrane in small defects and after tympanoplasty [13]. The use of PRT to seal the space around the prosthesis during piston stapedoplasty reduces the risk of developing sensorineural hearing loss in comparison with the use of adipose tissue or free position of the prosthesis. At the same time, the likelihood and intensity of ear noise decreases after piston stapedoplasty [7].
Based on the studies carried out in patients with chronic suppurative otitis media with the use of PRP while performing sanitizing surgery and tympanoplasty as a support for the nontympanic graft, faster healing of the postoperative cavity, restoration of hearing [3], and the use of PRP prevents the occurrence of perforations, atrophic changes membranes and the development of the adhesive process in the newly formed tympanic cavity [9].
As a result of an experimental study of the functional state of the sound-conducting system of the middle ear and morphological changes in the tympanic cavity after filling it with PRP in 6 pigs, the preservation of the ventilation function of the auditory tube, complete elimination of the clot from the tympanic cavity, without the formation of scars and adhesions was determined [8].
Obliteration of the frontal sinus with a tibia graft and the introduction of PRP after lavage and curettage of the sinus can be an effective treatment for chronic osteomyelitis of the frontal sinus [22].
The use of fibrin glue is more effective than tamponade of the nasal cavity with a hemostatic sponge, as well as the use of chemical and diathermocoagulation in patients with nosebleeds [32].
However, with the use of PRP after endonasal endoscopic surgery, no beneficial effect was found, the study was terminated early [28].
Rhinoplastic and septoplastic surgeries performed in 257 patients using protein-platelet convolutions from platelet-rich plasma showed their significant advantage over other covering materials [1].
Local application of PRP after tonsillectomy can significantly reduce the likelihood of postoperative bleeding, reduce the intensity of pain in the pharynx, and also reduce bacterial contamination of the wound surface in the pharynx, accelerating the process of tissue regeneration [15].
Conclusions: Thus, OLT is a new biotechnology in clinical practice. The safety and effectiveness of its use are widely covered in the literature, but many unresolved questions remain. Based on the analysis of scientific publications, a new step from a biological point of view, it is necessary to characterize the cellular composition of the final product (the presence of leukocytes, the number of platelets, etc.), which can affect the process of tissue regeneration. The possibility of systematizing the protocols for obtaining PRP will facilitate their use in daily clinical practice.
2. Bullanikov A.S., Semenov V.P. Increasing the efficiency of bone grafting with the use of platelet-rich plasma to replace defects in human bone tissue // Medical assistance. - 2007. - No. 1. - P.22-25.
3. Zavyalov FN, Goncharova OG The results of the use of autogenous platelet-rich plasma in patients who underwent middle ear surgery // Vestn. otorhinolaryngol. - 2011. - No. 1. - S. 28-30.
4. Ivanov P. Yu., Zhuravlev VP, Makeev OG The use of platelet-rich plasma for the prevention of jaw atrophy before dental implantation // Bulletin of the Ural Medical Academy of Sciences. - 2011. - No. 1. - S. 76-78.
5. Treatment of complications after operations on the abdominal organs using platelet-rich plasma / P.А. Popov, Yu.P. Popov, L.A. Magomedov [et al.] // Surgeon. - 2014. - No. 6. - S. 4-11.
6. Local therapy of gonarthrosis autologous platelet-rich plasma / L.Yu. Shirokova, S.M. Noskov, T.I. Bakhtiarova [et al.] // STM. - 2012. - No. 1. - S. 97-100.
7. Semenov F.V., Banashek-Meshcheryakova T.V. The use of platelet-rich plasma for the prevention of cochleovestibular disorders in piston stapedoplasty // Vestn. otorhinolaryngol. - 2011. - No. 3. - S. 47-50.
8. Semenov F.V., Banashek-Meshcheryakova T.V., Semenov V.F. Morphological and functional changes in the tympanic cavity after filling it with platelet-rich plasma (experimental study) // Vestn. otorhinolaryngol. - 2011. - No. 4. - S. 43-45.
9. Semenov FV Otoendoscopic evaluation of long-term results of tympanoplasty performed using platelet-rich plasma / FV Semenov // Ros. otorhinolaryngol. - 2013. - No. 3 (64). - S. 132-135.
10. Structural and functional features of the healing of aseptic wounds of soft tissues with the use of platelet-rich blood plasma / А.А. Glukhov, A.P. Ostroushko, S.N. Semenov [et al.] // Bulletin of experimental and clinical surgery. - 2010. - T. 3. - No. 3. - S. 210-213.
11. Technology "PlasmoliftingTM" - an injectable form of platelet autoplasma for the treatment of chronic periodontitis I – II severity / RR Akhmerov, MV Ovechkina, DE Tsyplakov [et al.] // Periodontology. - 2013. - No. 1. - S. 45-52.
12. Tolstov D. A., Bogdan V. G Platelet concentrates: classification, production technologies, biological effects / Minsk: BGMU, 2012. - P. 141-144.
13. Toropova L.A., Andriyanova I.V., Zhuikova T.V. Possibilities to restore the elasticity and integrity of the tympanic membrane using platelet-rich plasma / Mater. conf. otorhinolaryngol. and audiologists of FMBA, 28-29 November 2013, . // otorhinolaryngol. - adj. 2013 .-- P. 34.
14. The effectiveness of the use of platelet-rich plasma in the treatment of traumatic defects in the cartilage of the articular surfaces. Mastykov, V.P. Deikalo, I.V. Samsonova [et al.] // News of surgery. - 2013. - T. 21. - No. 4. - S. 3-9.
15. Yakobashvili I.Yu., Semenov F.V. The influence of local application of platelet-rich plasma on the course of the wound process after tonsillectomy // Ros. otorhinolaryngol. - 2008. - No. 4. - S. 26-30.
16. A comparative study of the effect of autologous platelet-rich plasma and fresh autologous whole blood on haemostasis after cardiac surgery / K. Yamamoto, J. Hayashi, H. Miyamura et al. // Cardiovasc. Surg. 1996; 4 (1): 9-14.
17. Comparison of the platelet concentrate collection system with the plasma-rich-in-growth-factors kit to produce platelet-rich plasma: a technical report / G. Weibrich, W. K. Kleis, W. E. Hitzler et al. // Int. J. Oral. Maxillofac. Implants. 2005; 20 (1): 118-123.
18. Current Knowledge and Perspectives for the Use of Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) in Oral and Maxillofacial Surgery. Part 2: Bone Graft, Implant and Reconstructive Surgery / A. Simonpieri, M. Del Corso, A. Vervelle [et al.] // Curr. Pharm. Biotechnol. 2012; 13: 1231-1256.
19. Determinants of Homologous Blood Usage Utilizing Autologous Platelet-Rich Plasma in Cardiac Operations / G. F. Giordano, G. F. Giordano Jr., S. L. Rivers et al. // Ann. Thorac. Surg. 1989; 47: 897-902.
20. Dohan Ehrenfest D.M., Rasmusson L., Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF) // Trends Biotechnol. 2009; 27: 158-167.
21. Efficacy of autologous platelet-rich plasma in thoracic aortic aneurysm surgery / I. Kashima, T. Ueda, H. Shimizu [et al.] // Jpn. J. Thorac. Cardiovasc. Surg. 2000; 48 (11): 708-712.
22. Frontal sinus obliteration using tibial bone graft and platelet-rich plasma for the treatment of chronic osteomyelitis / M. Acosta-Feria, P. Infante-Cossio, J. M. Hernandez-Guisado, et al. // Neurocirugia (Astur). 2006; 17 (4): 351-356; discus. 356.
23. Guner S., Buyukbebeci O. Analyzing the Effects of Platelet Gel on Knee Osteoarthritis in the Rat Model // Clin. Appl. Thromb. Hemost. 2013: 19 (5); 494-498.
24. Horowitz B, Busch M. Estimating the pathogen safety of manufactured human plasma products: application to fi brin sealants and to thrombin // Transfusion. 2008; 48: 1739-1753.
25. Man D., Plosker H., Winland-Brown J. E. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery // Plast. Reconstr. Surg. 2001; 107 (1): 229-237; disc. 238-239.
26. Mendonca-Caridad, J. J. Frontal sinus obliteration and craniofacial reconstruction with plateletrich plasma in a patient with fibrous dysplasia / J. J. Mendonca-Caridad, P. Juiz-Lopez, J. P. Rubio-Rodriguez // Int. J. Oral. Maxillofac. Surg.2006; 35 (1); 88-91.
27. Mishra A., Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma // Am. J. Sports Med. 2006; 34 (11): 1774-1778.
28. Rice D. H. Platelet-rich plasma in endoscopic sinus surgery / D. H. Rice // Ear. Nose Throat J. 2006; 85 (8): 516-518.
29. Rosenberg, E. S. Sinus grafting using platelet-rich plasma - initial case presentation / E. S. Rosenberg, J. Torosian // Pract. Periodont. Aesthet. Dent. 2000; 12 (9); 843-850; quiz 852.
30. Sonnleitner, D. A simplified technique for producing platelet-rich plasma and platelet concentrate for intraoral bone grafting techniques: a technical note / D. Sonnleitner, P. Huemer, D. Y. Sullivan // Int. J. Oral. Maxillofac. Implants. 2000; 15 (6): 879-882.
31. The role of leukocytes from L-PRP / L-PRF in wound healing and immune defense: new perspectives / T. Bielecki, D. M. Dohan Ehrenfest, P. A. Everts [et al.] // Curr. Pharm. Biotechnol. 2012; 13: 1153-1162.
32. Vaiman M., Segal S., Eviatar E. Fibrin glue treatment for epistaxis // Rhinology. 2002; 40 (2): 88-91.
33. What do we use: platelet-rich plasma or platelet-leukocyte gel? / P. A. Everts, A. van Zundert, J. P. A. M. Scho¨nberger [et al.] // J. Biomed. Mater. Res. 2008; 85: 1135-1136.